Emma Kotisalmi, Auli Hakulinen, Mika Mäkelä, Sanna Toppila-Salmi & Paula Kauppi
Research-Open Access
Asthma Research and Practice volume 6, Article number: 2 (2020)
Abstract
Background
Anti-IgE (omalizumab) and anti-IL5/IL5R (reslizumab, mepolizumab and benralizumab) treatments are available for severe allergic and eosinophilic asthma. In these patients, studies have shown beneficial effects in oral corticosteroid use and exacerbations. The aim of this retrospective single-center study was to evaluate the effect of biological therapy on severe asthma and to compare different therapies.
Methods
We collected and analysed results of anti-IL5/IL5R and anti-IgE therapies for asthma from January 2009 until October 2019 in specialized care. We compared number of exacerbations, asthma symptoms and use of per oral corticosteroids and antimicrobics because of asthma before and during biological therapy, and in a separate analysis need for per oral corticosteroids, antimicrobics or surgery due to upper respiratory tract diseases in asthmatics receiving biologicals. The analyses were done using the Chi square test, T-test or Mann-Whitney U -test, the Kruskall-Wallis test or the Wilcoxon test.
Results
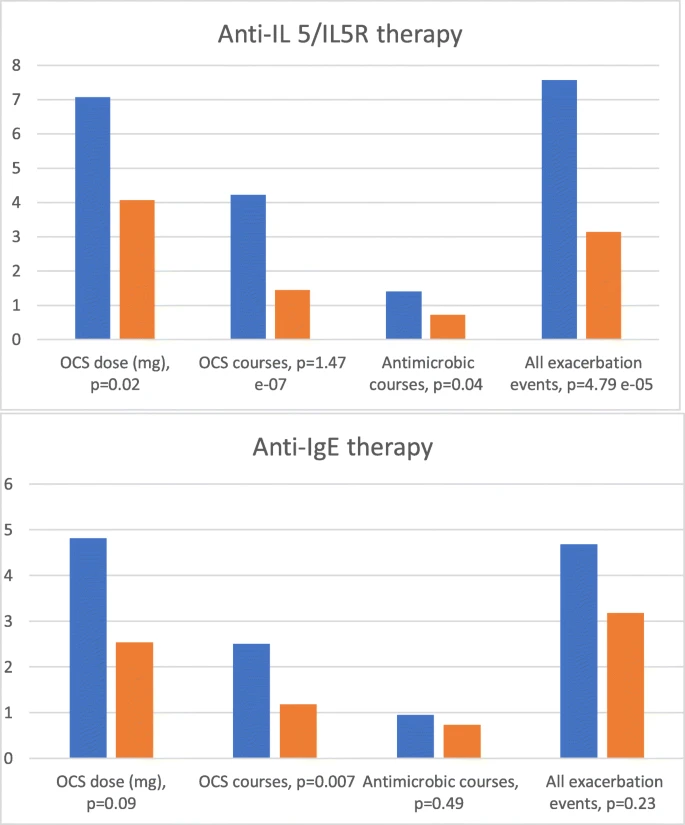
Of 64 patients, 40 used continuous per oral corticosteroid therapy prior to biological therapy. The mean daily dose of per oral corticosteroid was reduced in those with anti-IL5/IL5R therapy (− 3.0 mg, p = 0.02). The number of annual per oral corticosteroid courses decreased in both the anti-IL5/IL5R (− 2.8 courses, p < 0.05) and anti-IgE groups (− 1.3 courses, p < 0.05). The number of annual antibiotic courses (− 0.7 courses, p = 0.04) and total number of exacerbation events (− 4.4 events/year, p < 0.05) were reduced in the anti-IL5/IL5R group. In the 55 asthma patients analysed for upper respiratory tract findings, the results suggested a reduction in need for chronic rhinosinusitis surgery during biological therapy.
Conclusions
Results with biological therapies in this real-life clinical setting are comparable to those reported in clinical trials. Biological therapy reduces exacerbations and per oral corticosteroid use.
